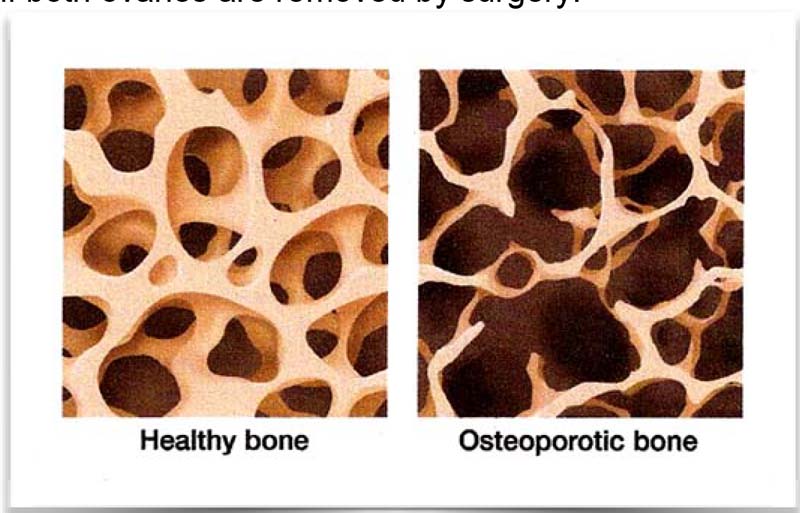
What is osteoporosis?
Osteoporosis occurs when the inside of the bones become porous and thin from a loss of calcium (see the picture below). This is called losing bone mass. Over time, this weakens the bones and makes them more likely to break.
Women are more likely to develop osteoporosis than men. This is due to several factors. Women have less bone mass than men, tend to live longer, take in less calcium, and need the female hormone estrogen to keep their bones strong. If men live long enough, they are also at risk of getting osteoporosis later in life.
Once total bone mass has peaked — around 35 years of age — all adults start to lose it. In women, the rate of bone loss speeds up after menopause, when estrogen levels fall. Since the ovaries make estrogen, faster bone loss may also occur if both ovaries are removed by surgery.
What are the risk factors for osteoporosis?
The following things put you at an increased risk for osteoporosis. The more of the following that apply to you, the higher your risk. Talk to your family doctor about your risk factors.
• Early menopause (before age 45)
• Family history of osteoporosis
• Surgery to remove ovaries before menopause
• Fair skin (Caucasian or Asian race)
• Not getting enough calcium in your food
• Sedentary lifestyle (not getting enough exercise)
• Smoking or tobacco use
• Excessive alcohol intake (more than three drinks a day)
• Excessive caffeine intake
• Eating disorders such as anorexia nervosa
• Thin body and small bone frame
• Hyperthyroidism, either from an overactive thyroid or from taking too much medicine to treat hypothyroidism
• Long-term use of corticosteroids, which are medicines prescribed to treat inflammation, pain and chronic conditions such as asthma and rheumatoid arthritis.
What are the signs of osteoporosis?
You may not know you have osteoporosis until you have serious signs. Signs include frequent broken bones or fractures of the wrist or hip, low back pain or a hunched back. You may also get shorter over time because osteoporosis can cause your vertebrae (the bones in your spine) to collapse. These are called compression fractures and can cause severe back pain. These problems tend to occur after a lot of bone calcium has already been lost.
How is osteoporosis diagnosed?
If your doctor suspects osteoporosis, he or she may suggest you have your bone mineral density (BMD) measured. A common test that measures bone density is called a dual energy X-ray absorptiometry (DEXA). This test measures BMD in your hips and spine, which are places likely to be affected by osteoporosis.
How is osteoporosis treated?
Treatment for osteoporosis starts with changes to your diet. You want to take in more calcium. Your doctor will suggest ways to get more calcium through food, drink and possibly a calcium supplement. He or she may also suggest you take a vitamin D supplement, which helps your body process calcium.
Your doctor will want you to increase your physical activity, especially weight-bearing exercise. This helps increase bone density. Examples of weight-bearing exercise include walking, jogging and climbing steps.
There are medicines available to treat osteoporosis. They include the following:
Bisphosphonates. These medicines help reduce the risk of breaks and fractures, as well as increase bone density in the hips and spine. They can be taken orally (in pill form) or intravenously (with an injection). Side effects include nausea, abdominal pain and irritation of the esophagus (the tube that connects the mouth to the stomach). People who cannot take bisphosphonates include people who have kidney disease, low levels of calcium in their blood and women who are pregnant or nursing. Examples of bisphosphonates are Alendronate (Fosamax), Risedronate (Actonel) and Ibandronate (Boniva).
Ibandronate is available as a pill or as an injection. If you take the pill, you have 2 options: a daily pill or a monthly pill (the pill you take each month has a greater dose of Ibandronate than the pill you take daily). If you take the injection, your doctor or nurse will give you a shot every 3 months. Some of the possible side effects include lower back or side pain, shortness of breath, tightness in the chest, and bloody or cloudy urine.
Calcitonin. This is a hormone that helps slow the breakdown of bone. It is available as an injection or nasal spray. Side effects include irritation of the lining of the nose and headache (with use of the nasal spray) and diarrhea, abdominal pain, nausea and vomiting (with use of the injection).
Raloxifene. This medicine is used to prevent and treat osteoporosis in women by increasing bone density. It is not a hormone, but it mimics some of the effects of estrogen. Side effects may include hot flashes and a risk of blood clots.
Teriparatide. This medicine is a synthetic form of parathyroid hormone and helps new bone to grow. It comes in an injectable form, and is injected once a day in the thigh or abdomen. It can be used in both women and men for the treatment of osteoporosis. Common side effects may include nausea, abdominal pain, headache, muscle weakness, fatigue and loss of appetite.
How much calcium do I need?
Before menopause, you need about 1,000 mg of calcium per day. After menopause, you need at least 1,200 mg of calcium per day. You should also aim for 800 to 1,000 international units (IU) of vitamin D each day (up to 2,000 IU daily is safe) to help your body absorb the calcium.
It’s usually best to try to get calcium from food. Non-fat and low-fat dairy products are good sources of calcium. Other sources of calcium include dried beans, pink salmon, spinach and broccoli.
About 300 mg of calcium are in each of the following: 1 cup of non-fat or low-fat yogurt, 1 1/2 cups of white beans, 5 ounces of salmon, 1/2 cup of spinach or 2 cups of broccoli.
If you don’t get enough calcium from the food you eat, your doctor may suggest taking a calcium supplement with Vitamin D. Take it at meal time or with a sip of milk, or as directed by your doctor or pharmacist.
Tips to keep bones strong
• Exercise.
• Eat a well-balanced diet with at least 1,200 mg of calcium a day.
• Quit smoking. Smoking makes osteoporosis worse.
• Talk to your doctor about hormone therapy (HT) and other medicines to prevent or treat osteoporosis.
* References from the patient education material of AAFP and CFPC.