I think it is safe to say we are all feeling a bit stressed these days. Statistics Canada indicates that most Canadians have experienced a decline in mental well-being since the beginning of the COVID-19 pandemic (Statistics Canada, 2020). As such, it seems timely to bring awareness to mental health, mental illness, and how we can develop protective factors to buffer against mental health issues and mental illnesses. With so much attention being given to reducing the spread of infectious disease, this article will use a similar analogy for protecting our mental health.
Mental illness affects 1 in 5 Canadians directly each year (Canadian Mental Health Association, 2021), but indirectly affects us all. Recognizing that mental illness is in fact a disease, and not the result of poor decision making or life circumstance, we can apply a preventative model to diseases that impact our minds in the same way we do with diseases that impact the body. Just like Covid-19 doesn’t directly affect all Canadians, it has certainly affected us all indirectly. Not all Canadians affected by Covid-19 will find themselves in the ICU, but we know that some people will require serious medical attention. In the same way, not all Canadians experiencing mental illness will have a severe case, but some do. We understand that certain factors contribute to the severity of Covid-19 symptoms, and, in just the same way, certain factors will contribute to the severity of mental illness. Most importantly, we know that many Canadians recover from Covid-19, just as many people experiencing mental illness in their lifetime will too.
We have all become familiar with the Alberta Health Services preventative guidelines to reduce the spread of Covid-19, such as getting vaccinated, wearing a mask, distancing, etc. Since these guidelines will not help improve our mental health, I will propose an analogy to apply to the protection of our mental health. If we are to apply a Covid-like strategy to protecting our mental health, the most important steps we can take are preventative in nature, as mental health promotion truly is mental illness prevention. While we may never have a vaccine to keep us from developing a mental illness, we can manage our mental health, identify the factors that may put us in higher risk of developing a severe mental illness, and increase protective factors to reduce our risk.
Get vaccinated ~ Build Knowledge/Identify Support Networks
As stated previously, we may never have a vaccine that protects us from developing mental illness, but we can consider knowledge to be a protector of our mental health. Understanding what mental health is, what mental illness is, signs and symptoms, and when and how to access mental health resources can support positive mental health. Learning this information before mental illness develops in yourself or someone you know can be an excellent first step in staying safe. While knowledge might not necessarily prevent one from developing a mental illness, learning this information can help reduce our risk of experiencing severe mental illness and increase our ability to reach out and ask for help and support. Another protective factor to draw attention to is the importance of building a network of support. Research suggests that feeling connected to and supported by others through social support can buffer against stress and illness and could act as a metaphorical vaccine. A support network may include family members, friends, co-workers, people in our communities, even professionals like doctors and counsellors. Support networks do not necessarily need to be large; quality over quantity is key here. Support networks can provide emotional support, knowledge and helpful advice, different perspectives, and practical help. While we are identifying our own social networks, it is important to consider whose networks we may be a part of. Providing support to others is just as beneficial as being supported.
Wear a Mask ~ Employ a Trauma Informed Approach
The consensus of the purpose of mask-wearing is that “my mask protects you; your mask protects me,” and perhaps the mental health ‘mask’ can be our thoughts, actions, and behaviours toward others. Considering the growing division of people these days, if we are to focus our words and actions toward others to be kind, compassionate, and empathetic, could the risk of mental illness in others be reduced? If we can shift a negative outlook to one that is more optimistic, a judgemental attitude to one that is more understanding, or a punitive approach to be more compassionate, could this improve the general mood of a community from despair to repair?
Stay 6 Feet Apart ~ Set Boundaries
While distancing from others can be disastrous for our mental health, we can look at the 6-foot rule as the implementation of boundaries to protect our mental health. If we must stay physically distanced from others, it is essential that we stay socially close to our support networks. Research indicates that strong social support is linked to better mental and physical health outcomes, particularly for those experiencing illness of some type. Identifying our natural supports – family members, friends, peers, community members we are connected to – and maintaining healthy relationships with these people helps to lower our risk of developing illness and improves health outcomes in the presence of disease. That said, it is important to recognize when boundaries need to be put in place. People often talk about putting boundaries in place for maintaining a work-life balance, but there are times when we need to put boundaries in place for family members, friends, and others. The best way we can do this is by asking ourselves if the emotional energy we give is equal to the emotional energy we receive from spending time with a loved one. If our exchanges leave us feeling drained, tired, or unfulfilled, it is okay to put a social boundary in place. Say it with me: “It is okay to put a social boundary in place.” We may do this by asking first “When I say yes to others, am I saying no to myself?” If your answer is yes, this would indicate the need for social boundaries.
Avoid Crowds and Poorly Ventilated Areas ~ Avoid Toxic People and Places
Speaking of boundaries, our mental health analogy of avoiding crowds and poorly ventilated areas would be to place boundaries around toxic people and situations. While we may not be facing physical crowds of people, the poorly ventilated areas in the mental health realm arise through social media. What used to be a fun place to reconnect with old friends and not-so-humbly brag about our successes has now become a nasty arena of fake news and people who do not think twice when sharing unhelpful, hurtful, or downright rude opinions. While it might be difficult to avoid the social network crowds altogether, we can ‘ventilate’ our newsfeed by blocking or unfollowing those who put our mental health at risk, and Marie Kondo our newsfeed by only allowing content that sparks joy. Kittens and art work best for me but find what speaks to you.
Wash Your Hands Often ~ Practice Self-Care
The mental health equivalent of washing our hands often will be self-care. A term used frequently these days – especially in the mental health circles – self-care may look different for everyone but is something we must prioritize when considering our overall well-being. There are many ways we can do this. To find out what works best, we can create a unique self-care plan with strategies to take care of our bodies, minds, emotions and feelings, and our souls. Taking care of our bodies might look like being active, eating nourishing foods, drinking enough water, and getting a good night’s sleep. Taking care of our minds might look like reading an enjoyable book, learning a new skill, or practicing gratitude. Taking care of our emotions and feelings might include journaling, identifying our feelings and having healthy strategies to manage them, and allowing them to arise without judgement. Taking care of our souls might look like practicing mindfulness, connecting with others, and feeling a sense of connection to the greater world around us.
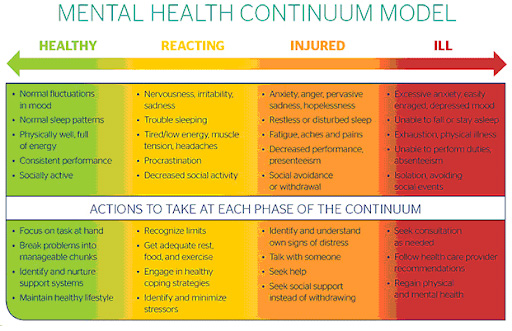
Monitor Health Daily ~ Make Use of the Mental Health Continuum Model
When it comes to monitoring our health daily, the mental health equivalent that comes to mind is to be aware of changes in our mental health and employ strategies to keep mental distress from worsening. The Mental Health Continuum Model (MHCM) is useful here as a self-help tool for identifying signs and symptoms of distress, and when we need additional support. The MHCM has four zones across a continuum with healthy functioning (the ‘Green Zone’) at one end, and clinically significant mental disorder (the ‘Red Zone’) at the other. Between the two points, we find mild and reversible distress (the ‘Yellow Zone’), and severe and persistent impairment (the ‘Orange Zone’). Looking at this through the Covid lens, we might see mild and reversible distress as symptoms that may or may not be Covid but require attention. A mental health ‘cough’ or ‘sneeze’ may shift us from healthy functioning into mild and reversible distress and can take the form of increased nervousness and worry, feeling overwhelmed, mild sleep disturbances, and greater vulnerability to stress. Tending to these symptoms might look like taking a mental health day from work, reducing your workload where possible, prioritizing sleep, and reaching out to a supportive loved one. Being aware of these changes and acting on them soon can help us return to the Green Zone and reduce our risk of moving into more severe impairment or serious illness.
If we notice that our ability to practice self-care or cope well with stress starts to diminish, we may find those mild, Yellow Zone symptoms worsening and having a greater impact on our day-to-day functioning. Shifting into the Orange Zone of severe and persistent impairment, we may find ourselves feeling more upset, frustrated, worried, or irritable than usual, noticeable changes in our sleep (difficulty falling and/or staying asleep, or wanting to sleep more than usual) and eating patterns (loss of appetite or eating larger amount of food than normal, even when not hungry), fatigue, lack of interest in activities previously enjoyed, and withdrawing from relationships for a period of at least two weeks, that cannot be explained by external circumstances (i.e. Unexpected job loss, death, or other external stressor).
If we are experiencing any of these symptoms, it is vital that we seek medical attention from a doctor or mental health professional as soon as possible to lower our risk of shifting into the severe mental illness zone. Reaching out for support from the professionals in our networks is key at this point. This zone of the MHCM could be equivalent to a hospital visit with Covid. Like those severe cases of Covid that lead to the ICU, some people experiencing clinical mental illness (the Red Zone) will need professional mental health support to return to healthy functioning. It is important to keep in mind that if we or a loved one are experiencing moderate to severe distress related to mental illness, there is help, and it is possible to recover from or live well with a diagnosed mental illness.
A visual of the Mental Health Continuum can be found at https://theworkingmind.ca/continuum-self-check
With this information in mind, mental health supports in Chestermere, Langdon, and South East Rocky View can be found via the Chestermere Area Mental Health Coalition Facebook page or https://www.yoursynergy.ca/wellnesssupport. Additional resources can be found on the City of Chestermere website here: https://www.chestermere.ca/mentalhealth.